|
|
|
| Extent and predictors of grade upgrading and downgrading in an Australian cohort according to the new prostate cancer grade groupings |
Kerri Beckmanna,b,*( ),Michael O’Callaghanc,d,Andrew Vincentd,Penelope Cohene,Martin Borgf,David Rodera,Sue Evansg,Jeremy Millarg,Kim Morettia,d ),Michael O’Callaghanc,d,Andrew Vincentd,Penelope Cohene,Martin Borgf,David Rodera,Sue Evansg,Jeremy Millarg,Kim Morettia,d
|
a Cancer Research Institute, School of Health Sciences, University of South Australia, Adelaide, Australia
b School of Cancer and Pharmaceutical Sciences, King's College London, London, UK
c Flinders Medical Centre, Urology Unit, Adelaide, Australia
d School of Medicine, University of Adelaide, Adelaide, Australia
e SA Pathology, Health SA, Adelaide, South Australia, Australia
f Genesis Care, University of Adelaide, Adelaide, Australia
g Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia |
|
|
|
|
Abstract Object: To determine the extent and impact of upgrading and downgrading among men who underwent radical prostatectomy (RP) according to new grade groupings and to identify predictors of upgrading from biopsy grade Group I and II, and downgrading to grade Group I, in a community setting. Methods: Study participants included 2279 men with non-metastatic prostate cancer diagnosed 2006-2015 who underwent prostatectomy, from the multi-institutional South Australia Prostate Cancer Clinical Outcomes Collaborative registry. Extent of up- or down-grading was assessed by comparing biopsy and prostatectomy grade groupings. Risk of biochemical recurrence (BCR) with upgrading was assessed using multivariable competing risk regression. Binomial logistic regression was used to identify pre-treatment predictors of upgrading from grade Groups I and II, and risk group reclassification among men with low risk disease. Results: Upgrading occurred in 35% of cases, while downgrading occurred in 13% of cases. Sixty percent with grade Group I disease were upgraded following prostatectomy. Upgrading from grade Group I was associated with greater risk of BCR compared with concordant grading (Hazard ratio: 3.1, 95% confidence interval: 1.7-6.0). Older age, higher prostate-specific antigen levels (PSA), fewer biopsy cores, higher number of positive cores and more recent diagnosis predicted upgrading from grade Group I, while higher PSA and clinical stage predicted upgrading from grade Group II. No clinical risk factors for reclassification were identified. Conclusion: Biopsy sampling errors may play an important role in upgrading from grade Group I. Improved clinical assessment of grade is needed to encourage greater uptake of active surveillance.
|
|
Received: 02 May 2018
Available online: 07 March 2019
|
|
Corresponding Authors:
Kerri Beckmann
E-mail: kerri.beckmann@unisa.edu.au
|
|
|
| Characteristic | Biopsy grade grouping | p-Valuea | | Grade I | Grade II | Grade III | Grade IV | Grade V | | Gleason pattern | 3 + 3 | 3 + 4 | 4 + 3 | 8 | 9-10 | | | N = 2272 | | Total, n (%) | 762 (34) | 821 (36) | 417 (18) | 193 (9) | 79 (3) | | | Clinical characteristics | | Age, year (mean ± SD) | 61 ± 7 | 63 ± 6 | 64 ± 7 | 65 ± 5 | 66 ± 5 | <0.001 | | PSA, ng/mL (IQR) | 7 (5-9) | 7 (5-10) | 8 (6-10) | 7 (6-11) | 8 (6-13) | <0.001 | | Public patient, n (%) | 264 (35) | 243 (30) | 100 (24) | 62 (32) | 27 (34) | 0.06 | | No. biopsy core (mean ± SD) | 13 ± 6 | 13 ± 6 | 14 ± 5 | 14 ± 7 | 14 ± 7 | 0.08 | | Re-biopsyb rate, n (%) | 123 (16) | 73 (9) | 37 (9) | 23 (12) | 4 (5) | <0.001 | | Outcomes | | PCa deathsc, n (%) | 3 (0.5) | 4 (0.7) | 3 (1.1) | 6 (4.3) | 4 (9.5) | <0.001 | | Other deathsc, n (%) | 17 (3) | 18 (3) | 9 (3) | 10 (7) | 2 (5) | 0.05 | | Biochemical recurrenced, n (%) | 59 (10) | 105 (19) | 89 (38) | 54 (43) | 22 (56) | <0.001 |
|
|
Cohort characteristics by biopsy grade (new grade groupings).
|
| Primary RP cases, n=2272 | Biopsy grade grouping | | Grade I (3+3) | Grade II (3+4) | Grade III (4+3) | Grade IV (8) | Grade V (9-10) | Total | | n = 762 | n = 821 | n = 417 | n = 193 | n = 79 | | Grade I (3+3) | 306 (40) | 68 (8) | 4 (1) | 2 (1) | 0 | | | Grade II (3+4) | 386 (51) | 522 (64) | 113 (27) | 22 (11) | 4 (5) | | | Grade III (4+3) | 58 (8) | 198 (24) | 227 (54) | 74 (38) | 8 (10) | | | Grade IV (8) | 8 (1) | 18 (2) | 41 (10) | 60 (31) | 10 (13) | | | Grade V (9-10) | 4 (1) | 15 (2) | 32 (8) | 35 (18) | 57 (72) | | | Total upgraded | 456 (60) | 231 (28) | 73 (18) | 35 (18) | 0 (0) | 795 (35) | | Total downgraded | 0 (0) | 68 (8) | 117 (28) | 98 (51) | 22 (28) | 305 (13) |
|
|
Upgrading/downgrading of grade groupings among men who underwent radical prostatectomy, n (%).
|
|
|
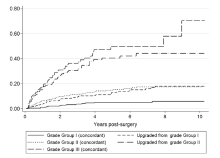
The crude cumulative incidence of biochemical recurrence following prostatectomy for men classified who were subsequently upgraded or downgraded in final surgical pathology.
|
| Grade category | SHR | 95% CI | p-Value | | Concordant BX- and RP-grade Group I | 1.0 | - | - | | Upgraded from BX-grade Group I | 3.1 | 1.7-6.0 | <0.001 | | Concordant BX- and RP-grade Group II | 3.6 | 1.9-6.9 | <0.001 | | Upgraded from BX-grade Group II | 9.4 | 5.0-17.9 | <0.001 | | Concordant BX- and RP-grade Group III | 11.8 | 6.1-22.6 | <0.001 |
|
|
Risk of biochemical recurrence upgraded cases relative to concordant grade Group I.
|
| Factors | Grade Group I (n = 735) | Grade Group II (n = 797) | | No. of upgraded/total | Adj. ORa | 95% CI | p-Value | No. of upgraded/total | Adj. ORa | 95% CI | p-Value | | Age at diagnosis (year) | | <55 | 80/139 | 1.2 | 0.7-1.9 | 0.45 | 22/91 | 0.8 | 0.4-1.4 | 0.35 | | 55-59 | 93/166 | 1.1 | 0.7-1.8 | 0.58 | 34/126 | 0.9 | 0.6-1.6 | 0.76 | | 60-64 | 104/195 | 1.0 | - | - | 56/209 | 1.0 | - | - | | 65-69 | 109/162 | 1.7 | 1.1-2.7 | 0.03 | 60/232 | 0.9 | 0.6-1.4 | 0.58 | | 70+ | 52/73 | 2.0 | 1.1-3.7 | 0.02 | 50/139 | 1.5 | 0.9-2.4 | 0.10 | | Pre-treatment PSA ng/mL | | <10 | 328/570 | 1.0 | - | - | 135/538 | 1.0 | - | - | | 10-19.9 | 73/107 | 1.6 | 1.0-2.6 | 0.04 | 46/134 | 1.6 | 1.1-2.1 | 0.02 | | ≥20 | 12/20 | 1.5 | 0.6-4.0 | 0.41 | 13/29 | 2.5 | 1.2-6.6 | 0.02 | | Not reported | 38/58 | 1.1 | 0.5-2.1 | 0.87 | 28/96 | 1.4 | 0.8-2.3 | 0.22 | | Clinical T stage | | ≤T2a | 179/318 | 1.0 | - | - | 60/247 | 1.0 | - | - | | T2b/c | 144/225 | 1.0 | 0.7-1.5 | 0.99 | 97/324 | 1.4 | 1.0-2.9 | 0.08 | | T3 | - | - | - | - | 13/23 | 5.1 | 2.0-12.9 | 0.001 | | Not reported | 115/192 | 1.0 | 0.7-1.6 | 0.81 | 52/203 | 1.1 | 0.7-1.7 | 0.74 | | Peri-neural invasion | | No evidence | 302/503 | 1.0 | - | - | 128/483 | 1.0 | - | - | | Yes | 48/79 | 1.0 | 0.6-1.7 | 0.94 | 71/248 | 1.2 | 0.8-1.6 | 0.51 | | Not reported | 96/153 | 1.4 | 0.9-2.1 | 0.11 | 23/66 | 1.7 | 0.9-3.0 | 0.09 | | Biopsy procedure | | TRUS | 425/707 | 1.0 | - | - | 211/247 | 1.0 | - | - | | Trans-perineal | 13/28 | 0.8 | 0.5-1.4 | 0.40 | 11/32 | 1.2 | 0.7-1.9 | 0.52 | | No. of biopsy cores | | ≤6 | 59/97 | 1.0 | - | - | 16/55 | 1.0 | - | - | | 7-11 | 110/204 | 0.7 | 0.4-1.3 | 0.24 | 66/225 | 1.2 | 0.6-2.3 | 0.68 | | 12-14 | 174/270 | 0.8 | 0.4-1.3 | 0.30 | 82/304 | 1.0 | 0.5-2.1 | 0.95 | | 15-18 | 62/99 | 0.5 | 0.3-1.0 | 0.06 | 31/122 | 1.0 | 0.4-2.2 | 0.95 | | ≥19 | 33/65 | 0.3 | 0.1-0.6 | 0.005 | 27/91 | 1.1 | 0.4-2.7 | 0.91 | | No. of positive cores | | ≤2 | 163/309 | 1.0 | - | - | 35/136 | 1.0 | - | - | | 3-4 | 125/201 | 1.6 | 1.1-2.4 | 0.02 | 65/230 | 1.1 | 0.7-1.8 | 0.71 | | 5-7 | 106/168 | 1.5 | 1.0-2.3 | 0.07 | 77/267 | 1.1 | 0.7-1.8 | 0.69 | | ≥8 | 44/59 | 2.3 | 1.2-4.7 | 0.02 | 24/164 | 0.9 | 0.5-1.6 | 0.68 | | Diagnosis year (continuous) | - | 1.2 | 1.1-1.3 | 0.001 | - | 1.0 | 0.9-1.0 | 0.43 |
|
|
Factors predicting risk of upgrading from biopsy grade Group I and grade Group II.
|
| Factors (Low risk disease only n = 409) | No. reclassified/total | Adj. ORa | 95% CI | p-Value | | Age at diagnosis (cont.) | 60/409 | 1.0 | 1.0-1.1 | 0.80 | | Year diagnosis (cont.) | - | 1.0 | 0.9-1.1 | 0.54 | | Pre-treatment PSA ng/mL (cont.) | - | 1.1 | 1.0-1.3 | 0.11 | | Grade Group | | - I | 25/260 | 1.0 | - | - | | - II | 35/149 | 2.9 | 1.6-5.3 | | | Clinical stage | | - T1c | 18/156 | 1.0 | - | - | | - T2 | 42/253 | 1.5 | 0.8-2.9 | 0.22 | | No. cores taken (cont) | - | 1.0 | 1.0-1.1 | 0.58 | | Percent positive cores | | - <10 | 8/91 | 1.0 | - | - | | - 10 to <15 | 13/81 | 1.7 | 0.7-4.6 | 0.26 | | - 15 to <20 | 22/100 | 2.1 | 1.0-5.2 | 0.11 | | - 20 to <25 | 12/64 | 1.8 | 0.6-4.8 | 0.27 | | - 25 or more | 5/73 | 0.5 | 0.1-1.5 | 0.20 |
|
|
Factors associated with upgrading leading to reclassification of risk category among men with low risk prostate cancer at biopsy.
|
| [1] |
National Comprehensive Cancer Network. NCCN clinical proactice guidelines in oncology: prostate cancer. Washington, DC, USA: NCCN; 2015 [Accessed May 12, 2018].
|
| [2] |
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA , et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. J Am Med Assoc 1998; 280:969-74.
|
| [3] |
Cooperberg MR, Pasta DJ, Elkin EP, Litwin MS, Latini DM, Du Chane J , et al. The University of California, San Francisco Cancer of the prostate risk assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol 2005; 173:1938-42.
|
| [4] |
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA , et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 2016; 40:244-52.
|
| [5] |
Eggener SE, Badani K, Barocas DA, Barrisford GW, Cheng JS, Chin AI , et al. Gleason 6 prostate cancer: translating biology into population health. J Urol 2015; 194:626-34.
|
| [6] |
Ross HM, Kryvenko ON, Cowan JE, Simko JP, Wheeler TM, Epstein JI . Do adenocarcinomas of the prostate with Gleason score (GS) _6 have the potential to metastasize to lymph nodes? Am J Surg Pathol 2012; 36:1346-52.
|
| [7] |
Bruinsma SM, Bangma CH, Carroll PR, Leapman MS, Rannikko A, Petrides N , et al. Active surveillance for prostate cancer: a narrative review of clinical guidelines. Nat Rev Urol 2016; 13:151-67.
|
| [8] |
Sandhu GS, Andriole GL . Active surveillance for prostate cancer: barriers to widespread adoption. Eur Urol 2012; 62:984-5.
|
| [9] |
Epstein JI, Feng Z, Trock BJ, Pierorazio PM . Upgrading and downgrading of prostate cancer from biopsy to radical prostatectomy: incidence and predictive factors using the modified Gleason grading system and factoring in tertiary grades. Eur Urol 2012; 61:1019-24.
|
| [10] |
Schreiber D, Wong AT, Rineer J, Weedon J, Schwartz D . Prostate biopsy concordance in a large population-based sample: a surveillance, epidemiology and end results study. J Clin Pathol 2015; 68:453-7.
|
| [11] |
Scattoni V, Maccagnano C, Capitanio U, Gallina A, Briganti A, Montorsi F . Random biopsy: when, how many and where to take the cores? World J Urol 2014; 32:859-69.
|
| [12] |
Beckmann K, Pinnock C, Tamblyn DJ, Kopsaftis T, Stapleton AM, Roder DM . Clinical and socio-demographic profile of an Australian multi-institutional prostate cancer cohort. Asia Pac J Clin Oncol 2009; 5:247-56.
|
| [13] |
Epstein JI, Allsbrook WC, Amin MB, Egevad LL, Committee IG . The 2005 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol 2005; 29:1228-42.
|
| [14] |
Stephenson AJ, Kattan MW, Eastham JA, Dotan ZA, Bianco FJ, Lilja H , et al. Defining biochemical recurrence of prostate cancer after radical prostatectomy: a proposal for a standardized definition. J Clin Oncol 2006; 24:3973-8.
|
| [15] |
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94:496-509.
|
| [16] |
StataCorp. Stata statistical software: release 12. College Station, TX: StatCorp LP; 2010.
|
| [17] |
Freedland SJ, Kane CJ, Amling CL, Aronson WJ, Terris MK, Presti JC , et al. Upgrading and downgrading of prostate needle biopsy specimens: risk factors and clinical implications. Urology 2007; 69:495-9.
|
| [18] |
Evans SM, Patabendi BV, Kronborg C, Earnest A, Millar J, Clouston D . Gleason group concordance between biopsy and radical prostatectomy specimens: a cohort study from prostate cancer outcome registrydvictoria. Prostate Int 2016; 4:145-51.
|
| [19] |
Moussa AS, Kattan MW, Berglund R, Yu C, Fareed K, Jones JS . A nomogram for predicting upgrading in patients with low- and intermediate-grade prostate cancer in the era of extended prostate sampling. BJU Int 2010; 105:352-8.
|
| [20] |
Moussa AS, Li J, Soriano M, Klein EA, Dong F, Jones JS . Prostate biopsy clinical and pathological variables that predict significant grading changes in patients with intermediate and high grade prostate cancer. BJU Int 2009; 103:43-8.
|
| [21] |
Corcoran NM, Casey RG, Hong MK, Pedersen J, Connolly S, Peters J , et al. The ability of prostate-specific antigen (PSA) density to predict an upgrade in Gleason score between initial prostate biopsy and prostatectomy diminishes with increasing tumour grade due to reduced PSA secretion per unit tumour volume. BJU Int 2012; 110:36-42.
|
| [22] |
Athanazio D, Gotto G, Shea-Budgell M, Yilmaz A, Trpkov K . Global Gleason grade groups in prostate cancer: concordance of biopsy and radical prostatectomy grades and predictors of upgrade and downgrade. Histopathology 2017; 70:1098-106.
|
| [23] |
Marra G, Eldred-Evans D, Challacombe B, Van Hemelrijck M, Polson A, Pomplun S , et al. Pathological concordance between prostate biopsies and radical prostatectomy using transperineal sector mapping biopsies: validation and comparison with transrectal biopsies. Urol Int 2017; 99:168-76.
|
| [24] |
Quintana L, Ward A, Gerrin SJ, Genega EM, Rosen S, Sanda MG , et al. Gleason misclassification rate is independent of number of biopsy cores in systematic biopsy. Urology 2016; 91:143-9.
|
| [25] |
Yang CW, Lin TP, Huang YH, Chung HJ, Kuo JY, Huang WJ , et al. Does extended prostate needle biopsy improve the concordance of Gleason scores between biopsy and prostatectomy in the Taiwanese population? J Chin Med Assoc 2012; 75:97-101.
|
| [26] |
Rosenkrantz AB, Taneja SS . Prostate MRI can reduce overdiagnosis and overtreatment of prostate cancer. Acad Radiol 2015; 22:1000-6.
|
| [27] |
Mizuno K, Inoue T, Kinoshita H, Yano T, Kawanishi H, Kanda H , et al. Evaluation of predictors of unfavorable pathological features in men eligible for active surveillance using radical prostatectomy specimens: a multi-institutional study. Jpn J Clin Oncol 2016; 46:1156-61.
|
| [28] |
Porcaro AB, Siracusano S, de Luyk N, Corsi P, Sebben M, Tafuri A , et al. Clinical factors stratifying the risk of tumor upgrading to high-grade disease in low-risk prostate cancer. Tumori 2018; 104:111-5.
|
| [29] |
Vora A, Large T, Aronica J, Haynes S, Harbin A, Marchalik D , et al. Predictors of Gleason score upgrading in a large African- American population. Int Urol Nephrol 2013; 45:1257-62.
|
| [30] |
Corcoran NM, Hong MK, Casey RG, Hurtado-Coll A, Peters J, Harewood L , et al. Upgrade in Gleason score between prostate biopsies and pathology following radical prostatectomy significantly impacts upon the risk of biochemical recurrence. BJU Int 2011; 108:e202-10.
|
| [31] |
Kinsella N, Helleman J, Bruinsma S, Carlsson S, Cahill D, Brown C , et al. Active surveillance for prostate cancer: a systematic review of contemporary worldwide practices. Transl Androl Urol 2018; 7:83-97.
|
| [32] |
de Cobelli O, Terracciano D, Tagliabue E, Raimondi S, Galasso G, Cioffi A , et al. Body mass index was associated with upstaging and upgrading in patients with low-risk prostate cancer who met the inclusion criteria for active surveillance. Urol Oncol 2015; 33:e1-8.
|
| [33] |
Porcaro AB, De Luyk N, Corsi P, Sebben M, Tafuri A, Cacciamani G , et al. Preoperative plasma levels of total testosterone associated with high grade pathology-detected prostate cancer: preliminary results of a prospective study in a contemporary cohort of patients. Curr Urol 2017; 10:72-80.
|
| [34] |
Ferro M, Lucarelli G, Bruzzese D, Di Lorenzo G, Perdona S, Autorino R , et al. Low serum total testosterone level as a predictor of upstaging and upgrading in low-risk prostate cancer patients meeting the inclusion criteria for active surveillance. Oncotarget 2017; 8:18424-34.
|
| [35] |
de Cobelli O, Terracciano D, Tagliabue E, Raimondi S, Bottero D, Cioffi A , et al. Predicting pathological features at radical prostatectomy in patients with prostate cancer eligible for active surveillance by multiparametric magnetic resonance imaging. PLoS One 2015;10:e0139696.
|
| [36] |
Futterer JJ, Briganti A, De Visschere P, Emberton M, Giannarini G, Kirkham A , et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol 2015; 68:1045-53.
|
| [37] |
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG . Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 2015; 68:438-50.
|
| [38] |
Barrett T, Haider MA . The emerging role of MRI in prostate cancer active surveillance and ongoing challenges. AJR Am J Roentgenol 2017; 208:131-9.
|
| [39] |
Tay KJ, Gupta RT, Holtz J, Silverman RK, Tsivian E, Schulman A , et al. Does mpMRI improve clinical criteria in selecting men with prostate cancer for active surveillance? Prostate Cancer Prostatic Dis 2017; 20:323-7.
|
| [40] |
Scott S, Samaratunga H, Chabert C, Breckenridge M, Gianduzzo T . Is transperineal prostate biopsy more accurate than transrectal biopsy in determining final Gleason score and clinical risk category? A comparative analysis. BJU Int 2015; 116:26-30.
|
| [41] |
Brimo F, Schultz L, Epstein JI . The value of mandatory second opinion pathology review of prostate needle biopsy interpretation before radical prostatectomy. J Urol 2010; 184:126-30.
|
| [1] |
Fubo Wang,Chao Zhang,Fei Guo,Xia Sheng,Jin Ji,Yalong Xu,Zhi Cao,Ji Lyu,Xiaoying Lu,Bo Yang. The application of virtual reality training for anastomosis during robot-assisted radical prostatectomy[J]. Asian Journal of Urology, 2021, 8(2): 204-208. |
| [2] |
Mengzhu Liu,Kun Jin,Shi Qiu,Pengyong Xu,Mingming Zhang,Wufeng Cai,Xiaonan Zheng,Lu Yang,Qiang Wei. Oncological outcomes of patients with ductal adenocarcinoma of the prostate receiving radical prostatectomy or radiotherapy[J]. Asian Journal of Urology, 2021, 8(2): 227-234. |
| [3] |
Maduwe Gedara Sagara Ruwan Kumara,Prasanga Thiranagama,Cherine Sosai,Anuruddha Abeygunasekera. A case of follicular cystitis treated successfully with diethylcarbamazine[J]. Asian Journal of Urology, 2021, 8(2): 235-237. |
| [4] |
Kulthe Ramesh Seetharam Bhat,Srinivas Samavedi,Marcio Covas Moschovas,Fikret Fatih Onol,Shannon Roof,Travis Rogers,Vipul R. Patel,Ananthakrishnan Sivaraman. Magnetic resonance imaging-guided prostate biopsy—A review of literature[J]. Asian Journal of Urology, 2021, 8(1): 105-116. |
| [5] |
Zepeng Jia,Yifan Chang,Yan Wang,Jing Li,Min Qu,Feng Zhu,Huan Chen,Bijun Lian,Meimian Hua,Yinghao Sun,Xu Gao. Sustainable functional urethral reconstruction: Maximizing early continence recovery in robotic-assisted radical prostatectomy[J]. Asian Journal of Urology, 2021, 8(1): 126-133. |
| [6] |
Anup Kumar,Vipul R. Patel,Sridhar Panaiyadiyan,Kulthe Ramesh Seetharam Bhat,Marcio Covas Moschovas,Brusabhanu Nayak. Nerve-sparing robot-assisted radical prostatectomy: Current perspectives[J]. Asian Journal of Urology, 2021, 8(1): 2-13. |
| [7] |
Michael C. Phung,Andrew R. Rouse,Jayce Pangilinan,Robert C. Bell,Erika R. Bracamonte,Sharfuddeen Mashi,Arthur F. Gmitro,Benjamin R. Lee. Investigation of confocal microscopy for differentiation of renal cell carcinoma versus benign tissue. Can an optical biopsy be performed?[J]. Asian Journal of Urology, 2020, 7(4): 363-368. |
| [8] |
Yang Chen,Tianyu Li,Jiwen Cheng. Ambiguous clear cell carcinoma in medullary sponge kidney: A case report[J]. Asian Journal of Urology, 2020, 7(4): 369-372. |
| [9] |
Simeng Wen,Yuanjie Niu,Haojie Huang. Posttranslational regulation of androgen dependent and independent androgen receptor activities in prostate cancer[J]. Asian Journal of Urology, 2020, 7(3): 203-218. |
| [10] |
Ieva Eringyte,Joanna N. Zamarbide Losada,Sue M. Powell,Charlotte L. Bevan,Claire E. Fletcher. Coordinated AR and microRNA regulation in prostate cancer[J]. Asian Journal of Urology, 2020, 7(3): 233-250. |
| [11] |
Yezi Zhu,Jun Luo. Regulation of androgen receptor variants in prostate cancer[J]. Asian Journal of Urology, 2020, 7(3): 251-257. |
| [12] |
Ramesh Narayanan. Therapeutic targeting of the androgen receptor (AR) and AR variants in prostate cancer[J]. Asian Journal of Urology, 2020, 7(3): 271-283. |
| [13] |
Yinghao Sun,Liping Xie,Tao Xu,Jørn S. Jakobsen,Weiqing Han,Per S. Sørensen,Xiaofeng Wang. Efficacy and safety of degarelix in patients with prostate cancer: Results from a phase III study in China[J]. Asian Journal of Urology, 2020, 7(3): 301-308. |
| [14] |
Anne Holck Storås,Martin G. Sanda,Olatz Garin,Peter Chang,Dattatraya Patil,Catrina Crociani,Jose Francisco Suarez,Milada Cvancarova,Jon Håvard Loge,Sophie D. Fosså. A prospective study of patient reported urinary incontinence among American, Norwegian and Spanish men 1 year after prostatectomy[J]. Asian Journal of Urology, 2020, 7(2): 161-169. |
| [15] |
Huan Chen,Bijun Lian,Zhenyang Dong,Yan Wang,Min Qu,Feng Zhu,Yinghao Sun,Xu Gao. Experience of one single surgeon with the first 500 robot-assisted laparoscopic prostatectomy cases in mainland China[J]. Asian Journal of Urology, 2020, 7(2): 170-176. |
|
|
|
|